What can go wrong?
As with all major surgical procedures, complications can occur. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following hamstring tendon graft reconstruction of the ACL are:
- anesthesia complications
- thrombophlebitis
- infection
- problems with the graft
- problems at the donor site
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include:
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following surgery, it is possible that the surgical incision can become infected. This will require antibiotics and possibly another surgical procedure to drain the infection.
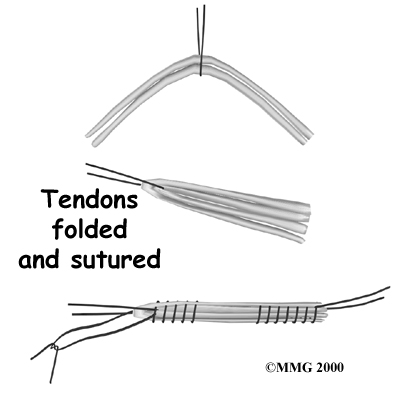
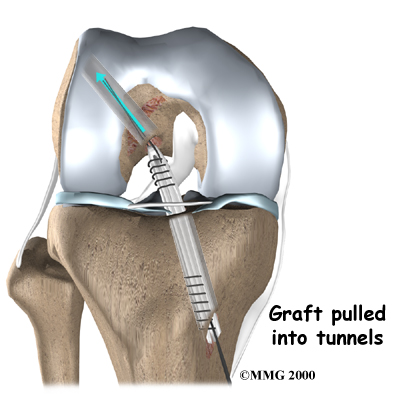
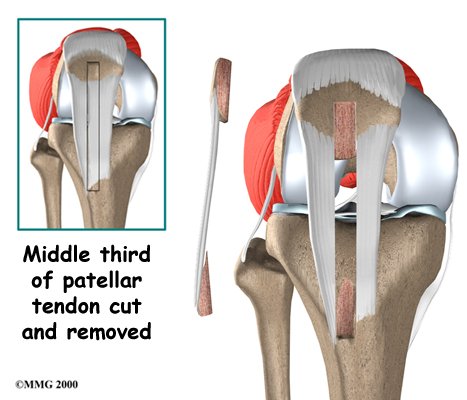
Problems with the Graft
After surgery, the body attempts to develop a network of blood vessels in the new graft. This process, called revascularization, takes about 12 weeks. The graft is weakest during this time, which means it has a greater chance of stretching or rupturing. A stretched or torn graft can occur if you push yourself too hard during this period of recovery. When revascularization is complete, strength in the graft gradually builds. A second surgery may be needed to replace the graft if it is stretched or torn.
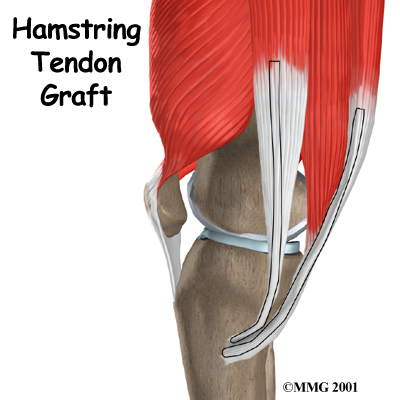
Problems at the Donor Site
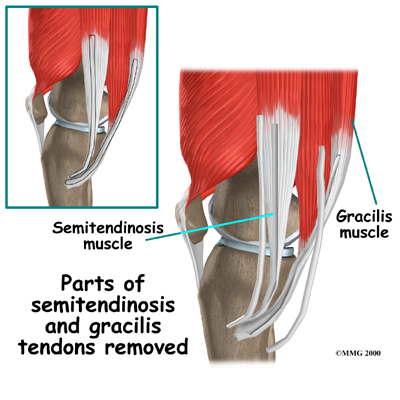
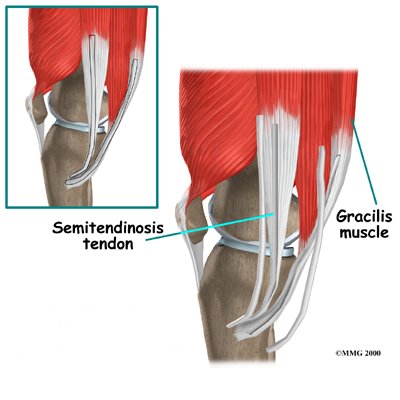
Problems can occur at the donor site (the area behind the leg where the hamstring graft was taken from the thigh). A potential drawback of taking out a piece of the hamstring tendon is a loss of hamstring muscle strength.
The main function of the hamstrings is to bend the knee (knee flexion). This motion may be slightly weaker in people who have had a hamstring tendon graft to reconstruct a torn ACL. Some studies, however, indicate that overall strength is not lost because the rest of the hamstring muscle takes over for the weakened area. Even the portion of muscle where the tendon was removed works harder to make up for the loss.
The hamstring muscles sometimes atrophy (shrink) near the spot where the tendon was removed. This may explain why some studies find weakness when the hamstring muscles are tested after this kind of ACL repair. However, the changes seem to mainly occur if both the semitendinosus and gracilis tendons were used. And the weakness is mostly noticed by athletes involved in sports that require deep knee bending. This may include participants in judo, wrestling, and gymnastics. These athletes may want to choose a different method of repair for ACL tears.
The body attempts to heal the donor site by forming scar tissue. This new tissue is not as strong as the original hamstring tendon. Because of this, there is a small chance of tearing the healing tendon, especially if the hamstrings are worked too hard in the early weeks of rehabilitation following surgery.


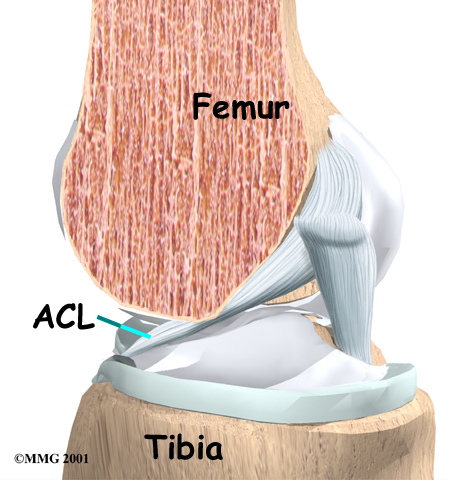
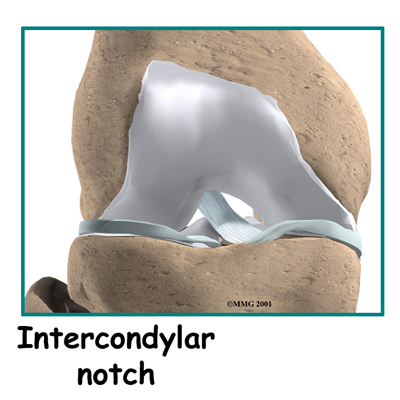

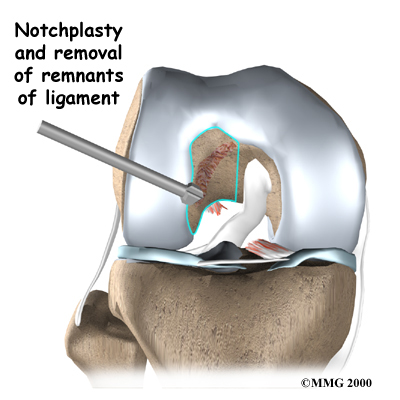
 The main goal of ACL surgery is to keep the tibia from moving too far forward under the femur bone and to get the knee functioning normally again.
The main goal of ACL surgery is to keep the tibia from moving too far forward under the femur bone and to get the knee functioning normally again.