Operative treatment can be broken down into several major categories, including 1) revascularization 2) intercarpal fusion; 3) lunate excision; 4) lunate decompression and joint-leveling procedures; 5) proximal row carpectomy; and 6) wrist fusion.
Revascularization
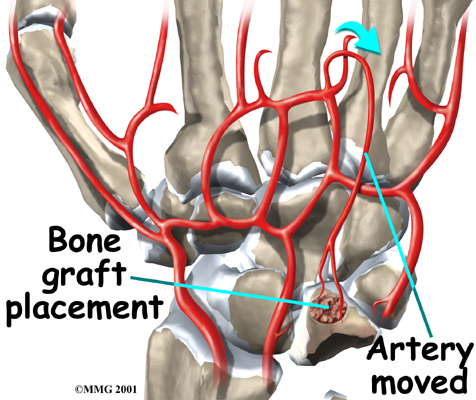 Stage two and stage three Kienbock's disease often require surgery when immobilizing the wrist doesn't help. Attempts to restore the blood flow to the lunate are most likely to be successful when the disease is in the early stages. The procedure to restore blood flow is called . During the operation, the surgeon moves a small section of blood vessels (and also possibly bone) from elsewhere on the wrist. The segment is attached to the deteriorating lunate bone. This is done to restore blood flow to the lunate and halt its deterioration. This is a newer procedure to treat Kienbock's disease and is not always successful. Vascularized bone graft does have the advantage of implanting live bone with a ready made blood supply.If this is successful, the bone heals and the blood supply in the transferred bone fragment grows into the rest of the lunate to restore the blood supply to the entire lunate.
Stage two and stage three Kienbock's disease often require surgery when immobilizing the wrist doesn't help. Attempts to restore the blood flow to the lunate are most likely to be successful when the disease is in the early stages. The procedure to restore blood flow is called . During the operation, the surgeon moves a small section of blood vessels (and also possibly bone) from elsewhere on the wrist. The segment is attached to the deteriorating lunate bone. This is done to restore blood flow to the lunate and halt its deterioration. This is a newer procedure to treat Kienbock's disease and is not always successful. Vascularized bone graft does have the advantage of implanting live bone with a ready made blood supply.If this is successful, the bone heals and the blood supply in the transferred bone fragment grows into the rest of the lunate to restore the blood supply to the entire lunate.
Intercarpal Fusion
Using an arthroscope, a thin instrument with a TV camera on the end, surgeons are able to operate using a small incision over the lunate. The surgeon cleans the area around the lunate, and then fuses the lunate to the carpal bone next to it. This is called an intercarpal fusion. It’s not a complete or total fusion because not all of the wrist bones are fused together. Bringing an extra blood vessel to revascularize the lunate (described above) is not necessarily a part of the treatment.
Lunate Excision
One of the oldest methods for treating Kienbock's disease is called a lunate excision. The abnormal bone was just removed, leaving an empty space in the wrist joint. The bones in the area collapsed into the empty space. This usually was not ideal and created problems later on. Other options include filling the empty space with a piece of tendon coiled up and stuffed into the hole. An artificial lunate bone may also be used to fill this space and maintain alignment of the bones.
Lunate Decompression and Joint Leveling
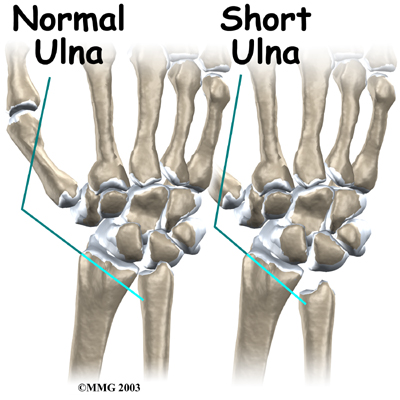
If you were born with an ulna that is too short, you have what is called an ulna minus wrist joint. As described above, this can lead to increased pressure on the lunate and may be contributing to the problem. Your surgeon may recommend a joint leveling procedure to reduce the pressure on the lunate. Doing this may allow the bone to heal and revascularize, or it may at least slow the progression of the arthritis in the joint. A joint leveling operation either shortens the bone that is too long ( the radius) or lengthens the bone that is too short (the ulna). Joint leveling operations include ulnar lengthening and radial shortening osteotomy.
Ulnar Lengthening
The operation for ulnar lengthening is done by making a small incision on the ulnar side of the wrist. The ulna bone is cut. Osteotomy is the term surgeons use to describe cutting a bone. The bone is not cut straight across, but like a stair step. This allows the surgeon to slide the two ends of the bone apart about 1/4 or 1/2 inch and still have the bone overlapping and connected. This type of cut prevents ending up with a large gap between the two segments of bone that can delay or prevent healing.
The surgeon will slide the two segments of ulna apart until X-rays show the joint is level and the radius and ulna are of equal length. The two segments of bone are held in place with a small metal plate and screws until they heal together. The plate may be removed once the bone heals.
Radial Shortening Osteotomy
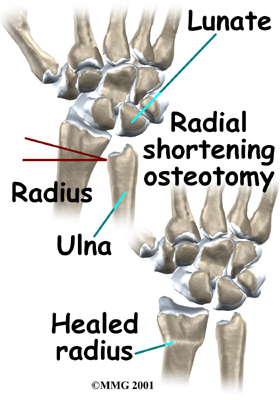
If your surgeon suggests a radial shortening osteotomy, then the goal is to shorten the bone that is too long. A radial osteotomy is sometimes preferred because the bone just heals better. The distal end of the radius near the wrist joint is larger than the ulna with a better blood supply. This means that it heals faster and more reliably.
To perform the radial osteotomy, the surgeon makes a small incision though the skin over the end of the radius. Before the operation, the surgeon uses the X-rays and measures how much bone must be removed to make the joint level. The radius is cut completely in two pieces and a small section, or wedge, of the bone near the wrist is removed. The two segments of the shortened radius are aligned and held in place with a metal plate and screws until healed. Some studies show this method has a lower rate of complications and good outcomes. It is used more often than ulnar lengthening.
 Stage two Kienbock’s disease and wrists in stage three that are stable can be treated with joint leveling procedures. Decreased pain with improved range of motion and strength are possible with joint leveling. But getting the exact length needed can be difficult.
Stage two Kienbock’s disease and wrists in stage three that are stable can be treated with joint leveling procedures. Decreased pain with improved range of motion and strength are possible with joint leveling. But getting the exact length needed can be difficult.
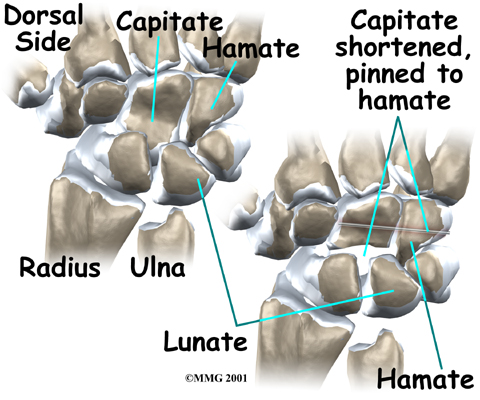
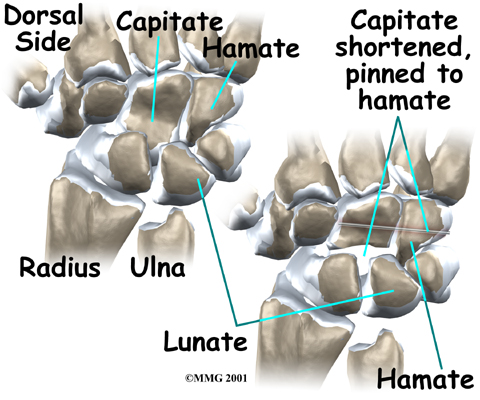
Capitate Shortening
Some surgeons prefer a (known as the Almquist procedure), which shortens a carpal bone on the other side of the lunate. Lunate decompression and capitate shortening are both helpful for reducing the force on the lunate. This procedure does not level the joint.
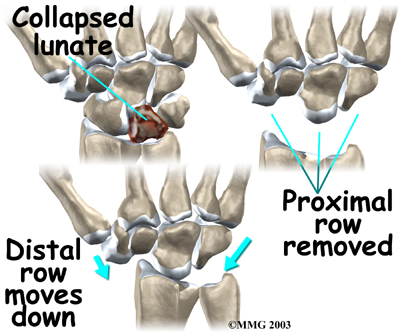
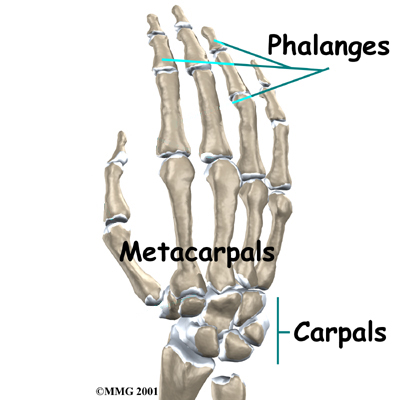
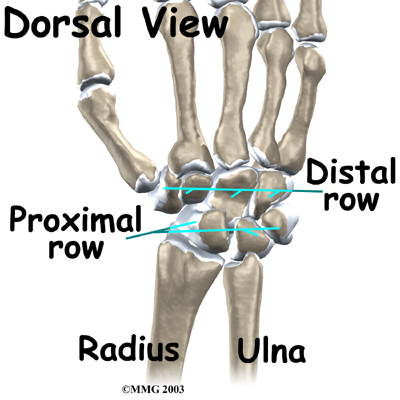
Carpectomy
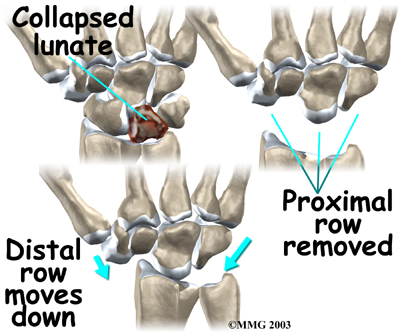
In stage four (late-stage) Kienbock's disease, surgeons focus on treating the wrist osteoarthritis that results when the lunate collapses and dies. One surgical option at this stage is proximal-row carpectomy. Carpectomy means excision (removal) of one or more of the carpal bones. The wrist is made up of two rows of carpal bones, four in each row. The lunate is in the proximal row (the row closest to the forearm). When the lunate has collapsed, but the wrist joint is not terribly arthritic, the four carpal bones of the proximal row may simply be removed. This allows the distal row (the other four bones) to slide down a bit and to begin moving against the forearm bones instead.
The wrist joint seems to work pretty well after this procedure. The advantage is that you will still have a good deal of wrist motion, unlike wrist fusion (described below). A proximal row carpectomy is a good solution when you need a flexible wrist more than you need a strong one, such as in someone who plays piano for a living.
During this procedure, the surgeon can also take out a section of the nerve that supplies feeling to the wrist joint to reduce wrist pain. This will not affect the feeling in your hand, because it only affects the nerve that goes to the wrist joint itself, below the skin level.
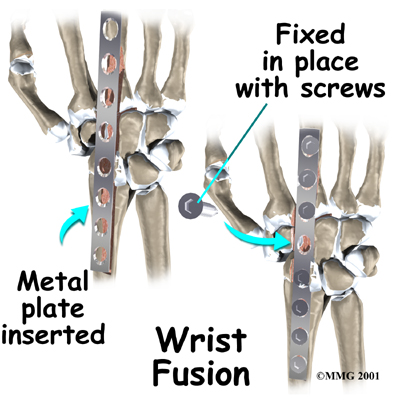
Wrist Fusion
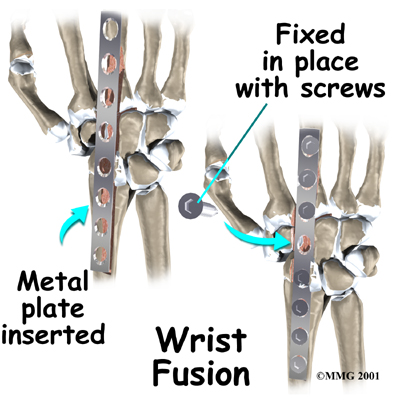
Finally, your surgeon may also suggest a wrist fusion when the entire wrist has become arthritic. (A wrist fusion is sometimes called an arthrodesis of the wrist). A fusion is an operation that allows all the bones of the wrist to grow together to form one bone. This makes the wrist stiff. You will not be able to bend the wrist after a fusion. You will be able to turn the wrist palm up and palm down. A fusion is a good solution when you need a strong wrist more than you need wrist movement, such as someone who does manual labor.
Related Document: Eastwood Physiotherapy's Guide to Wrist Fusion
Portions of this document copyright MMG, LLC.
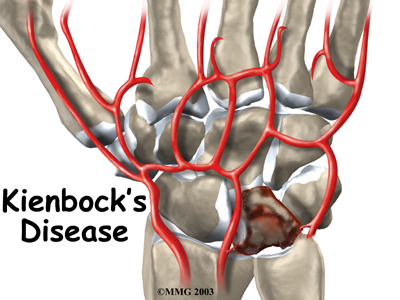


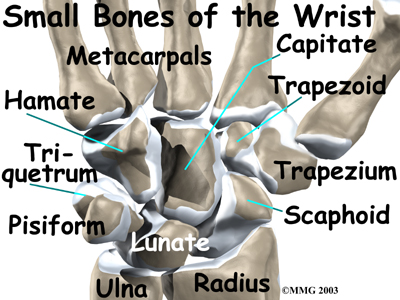
 The way that blood vessels supply the lunate is thought to play a role in Kienbock's disease. Some bones in the body simply have fewer blood vessels that bring in blood. The lunate is one of those bones. A bone with a limited blood supply may be more at risk of developing the disease after an injury. The reduced blood supply might be the result of a previous injury to the blood vessels.
The way that blood vessels supply the lunate is thought to play a role in Kienbock's disease. Some bones in the body simply have fewer blood vessels that bring in blood. The lunate is one of those bones. A bone with a limited blood supply may be more at risk of developing the disease after an injury. The reduced blood supply might be the result of a previous injury to the blood vessels.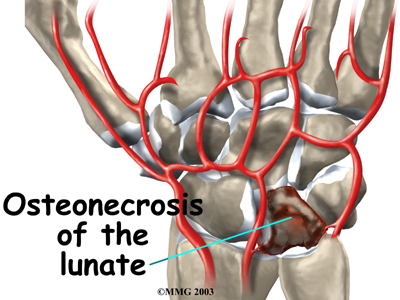

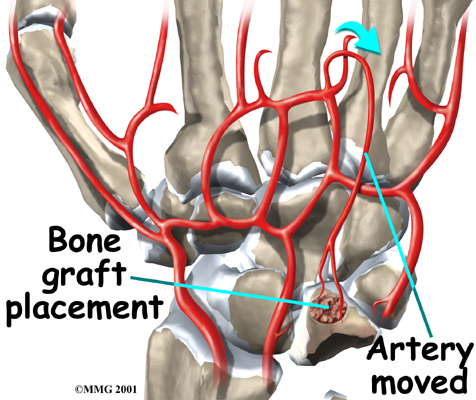 Stage two and stage three Kienbock's disease often require surgery when immobilizing the wrist doesn't help. Attempts to restore the blood flow to the lunate are most likely to be successful when the disease is in the early stages. The procedure to restore blood flow is called
Stage two and stage three Kienbock's disease often require surgery when immobilizing the wrist doesn't help. Attempts to restore the blood flow to the lunate are most likely to be successful when the disease is in the early stages. The procedure to restore blood flow is called 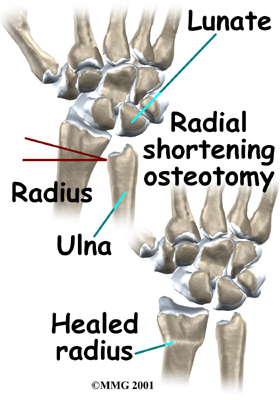
 Stage two Kienbock’s disease and wrists in stage three that are stable can be treated with joint leveling procedures. Decreased pain with improved range of motion and strength are possible with joint leveling. But getting the exact length needed can be difficult.
Stage two Kienbock’s disease and wrists in stage three that are stable can be treated with joint leveling procedures. Decreased pain with improved range of motion and strength are possible with joint leveling. But getting the exact length needed can be difficult.