What might go wrong?
All types of spine surgery, including artificial disc replacement, have certain risks and benefits. Weigh these as you gather advice and information. Be sure to discuss the possible risks of disc replacement with your spine surgeon.
Medical complications arising from spinal surgery are rare but could include stroke, heart attack, spinal cord or spinal nerve injury, pneumonia, or possibly death.
However, information from the disc replacement operations shows a low rate of complications. There have been no reports of death, significant infection, or major neurological problems.
As with all major surgical procedures, complications can occur. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications are:
- anesthesia complications
- thrombophlebitis
- infection
- blood loss
- nerve injury or paralysis
- spontaneous ankylosis (fusion)
- subsidence (sinking)
- implant failure (need for further surgery)
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin's surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Blood Loss
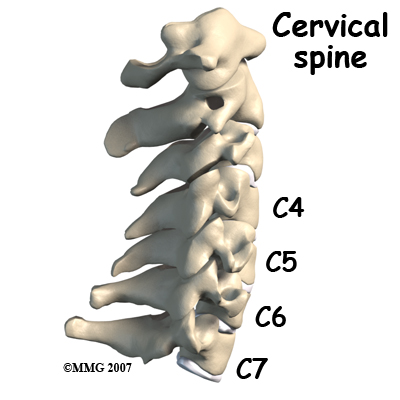
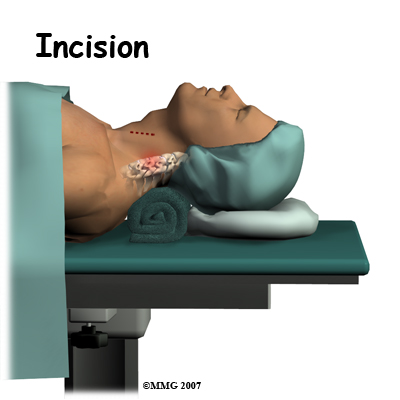
Cervical disc replacement surgery carries risks associated with operating from the front of the spine. Blood vessels that travel near the front of the spine may be injured during anterior cervical surgery.
Nerve Injury
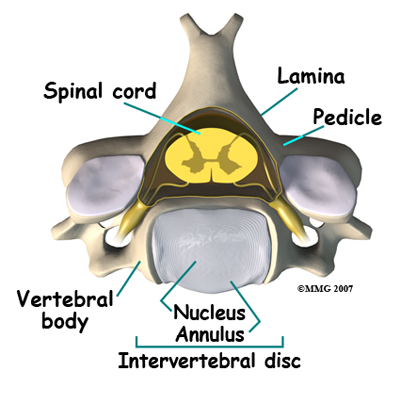
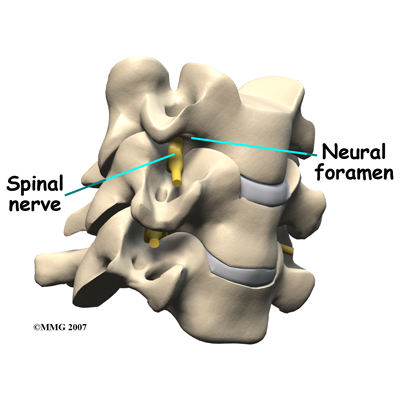
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
The nerve to the voice box is sometimes injured during surgery on the front of the neck. When doing anterior neck surgery, surgeons prefer to go through the left side of the neck where the path of the nerve to the voice box is more predictable than on the right side. During surgery, the nerve may get stretched too far when retractors are used to hold the muscles and soft tissues apart. When this happens, patients may be hoarse for a few days or weeks after surgery. In rare cases where the nerve is actually cut, patients may end up with ongoing minor problems of hoarseness, voice fatigue, or difficulty making high tones.
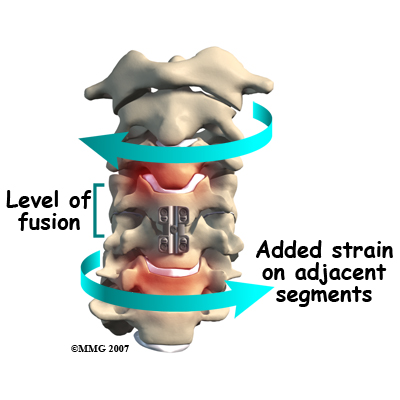
Spontaneous Ankylosis (fusion)
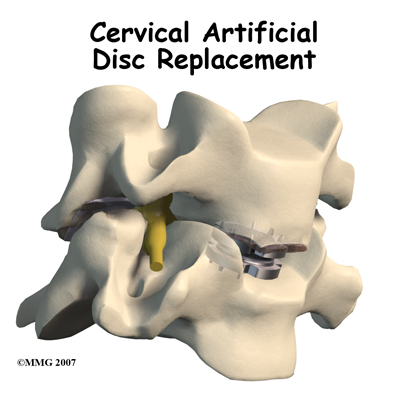
Some things can go wrong with any implant. In the case of artificial disc replacements for the cervical spine, sometimes the spine fuses itself, a process called spontaneous ankylosis. Loss of neck motion is the main side effect of this problem.
Bone may also form in the soft tissues around the vertebrae. For example, cartilage turns to bone or bone-like tissue. This process is called ossification. Ossification may not affect the implant or your final results in terms of motion or function.
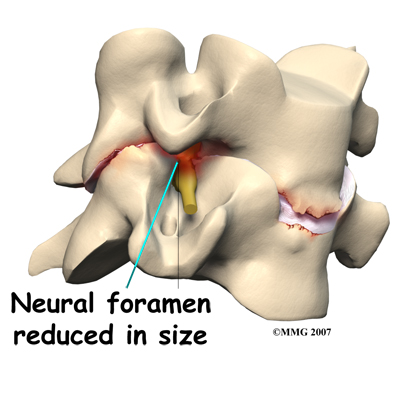
Some patients are left with pain, numbness, and weakness. This can occur when there’s been incomplete neurologic decompression. In other words, there is still pressure on the spinal cord or spinal nerves.
Subsidence (sinking)
Subsidence is another possible problem. The implant actually sinks down into the vertebral body above or below it. This results in a loss of the normal disc height. Neurologic compression with neurologic symptoms can occur.
Implant Failure (need for further surgery)
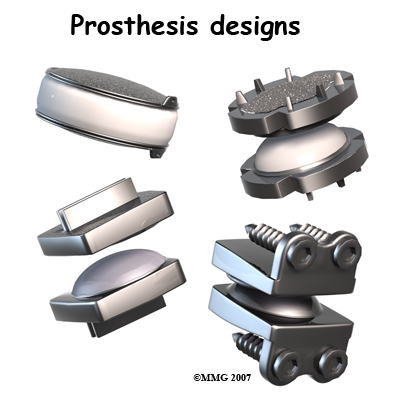
Over time, wear and tear just from the physical process of motion across a bearing surface can cause tiny bits of debris to flake off the implant. The body may react to these particles with an inflammatory response that can cause pain, implant loosening, and implant failure. So far, significant inflammatory reactions have not been reported for spinal artificial disc replacements. In rare cases, the artificial disc replacement can dislocate.
After Surgery
What happens after surgery
Most people spend one or two days in the hospital. You may require an extra day or two if for some reason you’re having extra pain or unexpected difficulty. Patients generally recover quickly after the artificial disc procedure.
You should be able to get out of bed and walk within a few hours. Move carefully and comfortably, and avoid extending your neck (bending backward). You may need to wear a brace or soft collar for a short while after the operation to support your neck muscles.
As you recover in the hospital, a physiotherapist may see you one or two times each day until you go home. You’ll be shown ways to move, dress, and do activities without putting extra strain on your neck. Your physiotherapist will help you begin a walking program in the hospital. You are encouraged to continue the walking program when you return home.
When you leave the hospital, there are very few activity restrictions. You should be safe to sit, walk, and drive. However, you should avoid lifting items for at least four weeks. Your surgeon will probably release you to return to work in two to four weeks. If your job requires moving and lifting heavy items, you may require a longer period of recovery. Your surgeon may give you the okay to do all your activities by the sixth week after surgery.
If you spend large amounts of time in front of a computer or other machine, you may need to change the height and angle of your work surface and/or the computer. Finding a position that puts minimal stress on your neck is important. You should avoid spending hours in one position reading, sewing, or doing other handwork. The physiotherapist can help you find optimal positions and advise you about ways to stretch your neck muscles.
Eastwood Physiotherapy provides services for physiotherapy in Edmonton.