What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following anterior lumbar fusion with cages include
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- blood vessel damage
- problems with the graft or hardware
- nonunion
- ongoing pain
This is not intended to be a complete list of the possible complications.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin's surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat. They may require additional surgery to treat the infected portion of the spine.
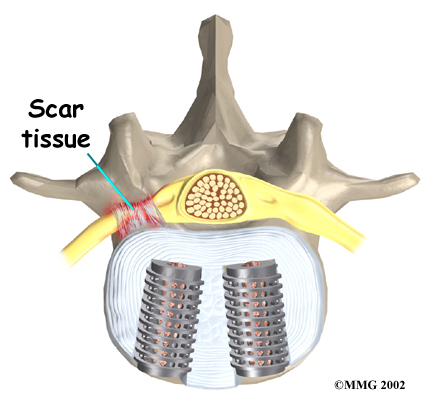
 Nerve Damage
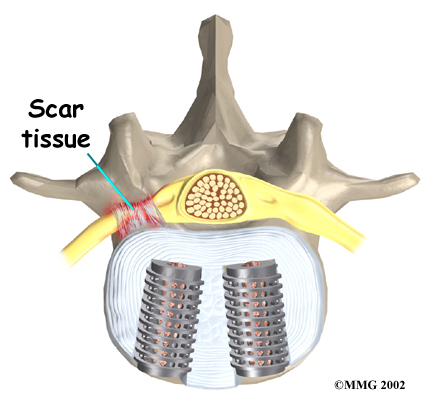
Nerve Damage
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of . An injury to the spinal cord or spinal nerves can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
Blood Vessel Damage
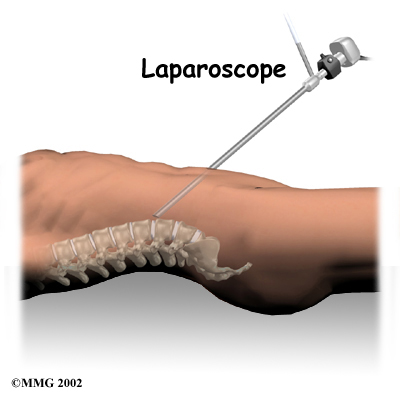
The abdominal aorta (the largest artery in the body) and the large veins that accompany it run in front of the spine as they split to run to each leg. These vessels must be moved aside to perform the anterior cage procedure. Because of this, the vessels may be injured, causing bleeding. When the procedure is performed using the laparoscope, too much bleeding may require opening the abdomen with a larger incision to repair the injured vessels.
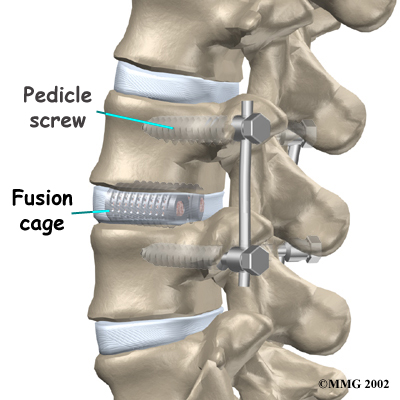
Problems with the Graft or Hardware
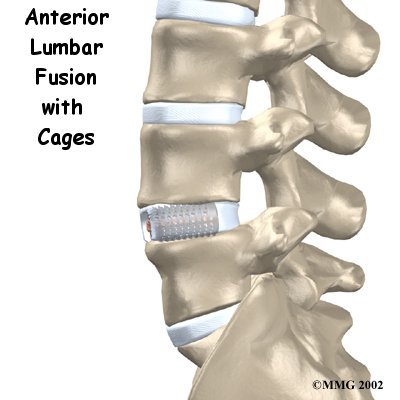
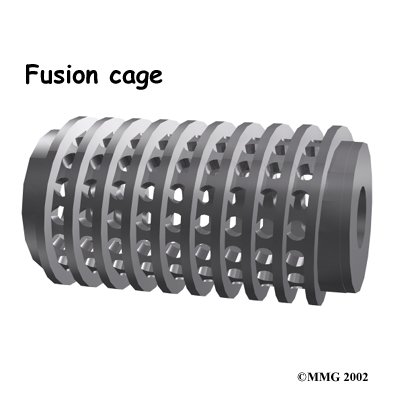
Fusion surgery with cages requires bone grafting. The graft is commonly taken from the top rim of the pelvis (autograft). As mentioned earlier, there is a risk of pain, infection, or weakness in the area where the graft is taken. These risks are avoided when a bone graft substitute, such as BMP-2, is used in place of an autograft.
After the cages are in place, the surgeon checks their position before completing the surgery. However, the cages may shift slightly soon after surgery to the point that they are no longer able to hold the spine stable. Abnormal or excessive loads on the spine, for example from heavy lifting or carrying or from the impact of jumping from a high surface, can cause the cages to collapse. This shifting or collapsing of the cages can cause injury to the nearby tissues. If this happens, a second surgery may be needed to replace the cages and to apply additional instrumentation to lock the spine firmly in place.
 Hardware can also cause problems. Screws or pins may loosen and irritate the nearby soft tissues. Also, the metal plates can sometimes break. If this happens, the surgeon may suggest another surgery either to take out the hardware or to add more hardware to solve the problem.
Hardware can also cause problems. Screws or pins may loosen and irritate the nearby soft tissues. Also, the metal plates can sometimes break. If this happens, the surgeon may suggest another surgery either to take out the hardware or to add more hardware to solve the problem.
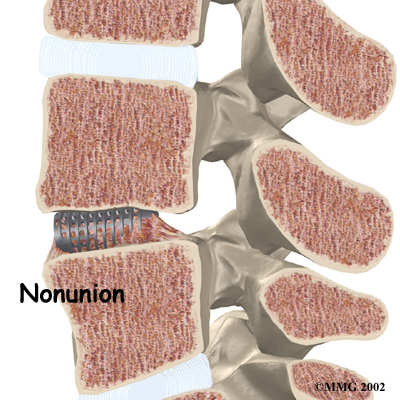
Nonunion
Sometimes the bones . This is called a nonunion, or pseudarthrosis. (The term pseudarthrosis means false joint.) When more than one level of the spine is fused at one time, there is a greater chance that nonunion will occur. Fusion of more than one level means two or more consecutive discs are removed and replaced with bone graft. If the joint motion from a nonunion causes pain, you may need a second operation.
In the second procedure, the surgeon may have to replace the cages. Metal plates and screws may also be added to rigidly secure the bones so they will fuse.
Ongoing Pain
Anterior lumbar fusion with cages is a complex surgery. Not all patients get complete pain relief with this procedure. As with any surgery, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.



 What happens during the operation?
What happens during the operation?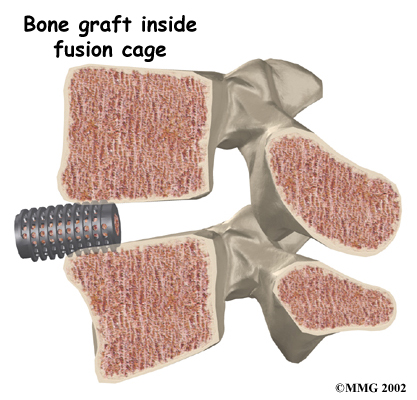
 Nerve Damage
Nerve Damage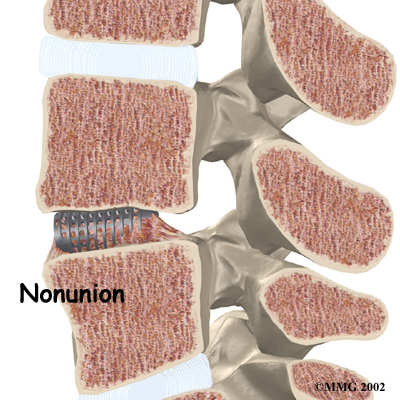 Hardware can also cause problems. Screws or pins may loosen and irritate the nearby soft tissues. Also, the metal plates can sometimes break. If this happens, the surgeon may suggest another surgery either to take out the hardware or to add more hardware to solve the problem.
Hardware can also cause problems. Screws or pins may loosen and irritate the nearby soft tissues. Also, the metal plates can sometimes break. If this happens, the surgeon may suggest another surgery either to take out the hardware or to add more hardware to solve the problem.