Non-surgical Rehabilitation
Whenever possible, nonsurgical treatment of lumbar degenerative disc disease is preferred. The first goal of nonsurgical treatment is to ease pain and other symptoms so the patient can resume normal activities as soon as possible.
We rarely prescribe bed rest for patients with degenerative disc problems. Instead, patients are encouraged to do their normal activities using pain as a gauge for how much is too much. If symptoms are severe, a maximum of typically two days of bed rest may be prescribed.
After evaluating your condition, your physiotherapist at Eastwood Physiotherapy can assign positions and exercises to ease symptoms. Our physiotherapist can design a personalized exercise program to improve flexibility of tight muscles, to strengthen the back and abdominal muscles, and to help you move safely and with less pain. Although recovery time varies among patients, as a guideline you may expect to work with our physiotherapist a few times each week for four to six weeks. In some cases, patients may need a few additional weeks of care.
Our first goal of treatment is to control symptoms. Your physiotherapist will work with you to find positions and movements that ease pain. We may use heat, cold, ultrasound, and electrical stimulation to calm pain and muscle spasm.
Our physiotherapist may perform hands-on treatments such as massage and specialized forms of soft-tissue mobilization. These can help a patient begin moving with less pain and greater ease. Traction is also a common treatment for degenerative disc problems. Traction gently stretches the low back joints and muscles. Our physiotherapist will instruct you on stretches that will help you move easier and with less pain.
As you recover, we will gradually advance you in a series of strengthening exercises for the abdominal and low back muscles. Working these core muscles helps patients move more easily and lessens the chances of future pain and problems.
A primary purpose of physiotherapy is to help you learn how to take care of your symptoms and prevent future problems. We’ll give you a home program of exercises to continue improve flexibility, posture, endurance, and low back and abdominal strength. Our physiotherapist will also discuss strategies you can use if your symptoms flare up.
Post-surgical Rehabilitation
Rehabilitation after surgery is more complex. Some patients leave the hospital shortly after surgery. However, some surgeries require patients to stay in the hospital for a few days.
During recovery from surgery, patients should follow their surgeon's instructions about wearing a back brace or support belt. You should be cautious about overdoing activities in the first few weeks after surgery.
Many surgical patients need physiotherapy outside of the hospital. Patients who've had lumbar fusion surgery normally need to wait up to three months before beginning a rehabilitation program. Our treatment sessions help patients build strength and learn to move and do routine activities without putting extra strain on their backs.
Although the length of Eastwood Physiotherapy rehabilitation programs vary based on an individual patient’s rate of recovery, as a guideline you can expect to attend physiotherapy sessions for eight to 12 weeks and should expect full recovery to take up to six months.
As your physiotherapy sessions come to an end, our physiotherapist will help you get back to the activities you enjoy. You may need guidance on which activities are safe or how to change the way you go about your activities. Ideally, patients are able to resume normal activities.
When recovery is well under way, regular visits to Eastwood Physiotherapy will end. Although we will continue to be a resource, you will be are in charge of doing your exercises as part of an ongoing home program.
Eastwood Physiotherapy provides services for physiotherapy in Edmonton.



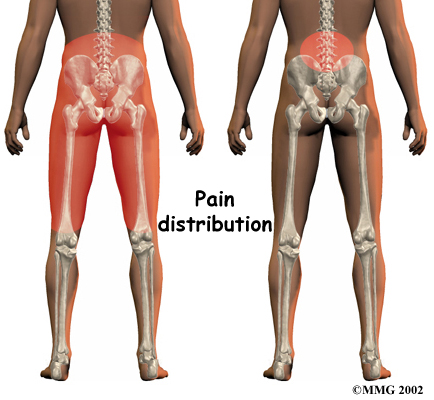 What does the condition feel like?
What does the condition feel like? Back braces are sometimes prescribed. Keeping the moving parts of the low back still can help calm mechanical pain. When a doctor issues a brace, he or she normally asks that the patient only wear it for two to four days. This lessens the chance that the trunk muscles will shrink (atrophy) from relying on the belt.
Back braces are sometimes prescribed. Keeping the moving parts of the low back still can help calm mechanical pain. When a doctor issues a brace, he or she normally asks that the patient only wear it for two to four days. This lessens the chance that the trunk muscles will shrink (atrophy) from relying on the belt.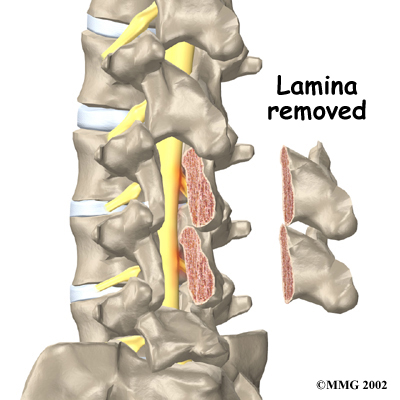 People with degenerative disc problems tend to gradually improve over time. Most do not need surgery. In fact, only one to three percent of patients with degenerative disc problems typically require surgery.
People with degenerative disc problems tend to gradually improve over time. Most do not need surgery. In fact, only one to three percent of patients with degenerative disc problems typically require surgery.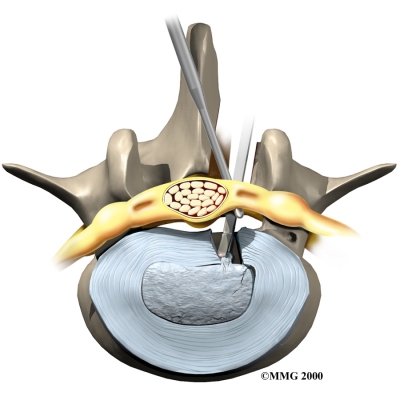 Discectomy
Discectomy