What could go wrong?
As with all major surgical procedures, complications can occur. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following hip resurfacing arthroplasty surgery include:
- anesthesia complications
- thrombophlebitis
- infection
- dislocation
- femoral neck fracture
- leg length inequality
- loosening
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
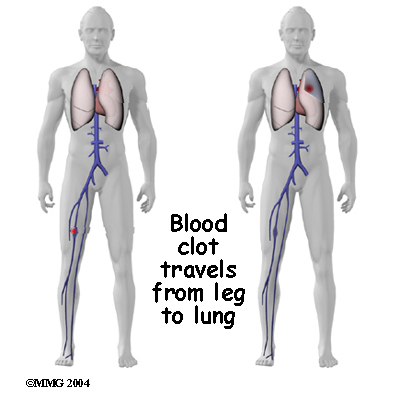
Thrombophlebitis (Blood Clots)
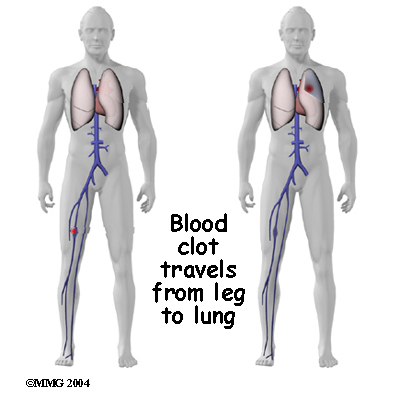
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include:
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection can be a very serious complication following artificial joint replacement surgery. The chance of getting an infection following hip joint resurfacing is probably around one percent. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want to make sure that you take antibiotics when you have dental work or surgical procedures on your bladder or colon to reduce the risk of spreading germs to the joint.
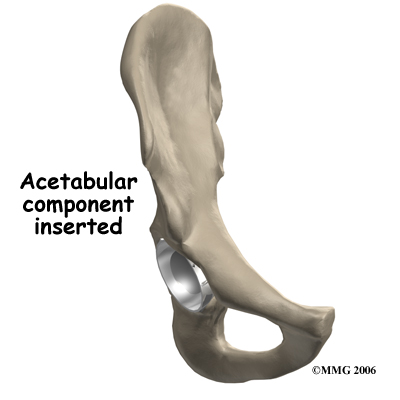
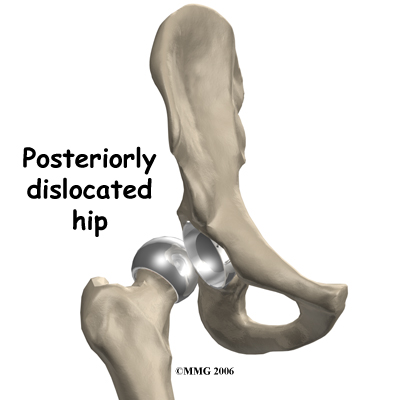
Dislocation
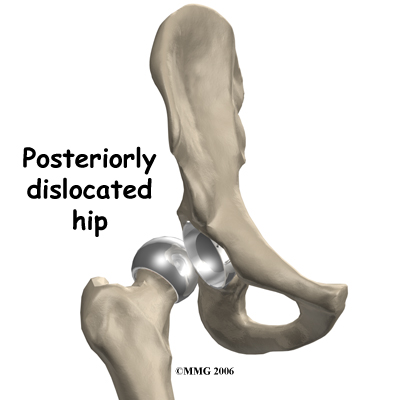
Just like your real hip, an artificial hip can dislocate if the ball comes out of the socket. There is a greater risk just after surgery, before the tissues have healed around the new joint, but there is always a risk. The physiotherapist will instruct you very carefully how to avoid activities and positions that may have a tendency to cause a hip dislocation. A hip that dislocates more than once may have to be revised to make it more stable. This means another operation.
Related Document: Eastwood Physiotherapy's Guide to Artificial Hip Dislocation Precautions
Loosening
The main reason that artificial joints eventually fail continues to be the loosening of the metal or cement from the bone. Great advances have been made in extending how long an artificial joint will last, but most will eventually loosen and require a revision. Hopefully, you can expect 12 to 15 years of service from an artificial hip, but in some cases the hip will loosen earlier than that. A loose hip is a problem because it causes pain. Once the pain becomes unbearable, another operation will probably be required to revise the hip.
Related Document: Eastwood Physiotherapy's Guide to Revision Arthroplasty of the Hip
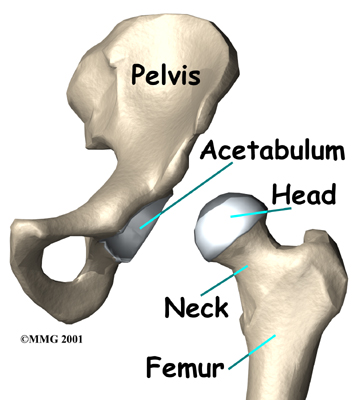
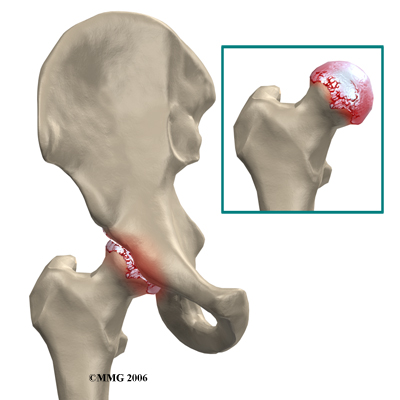
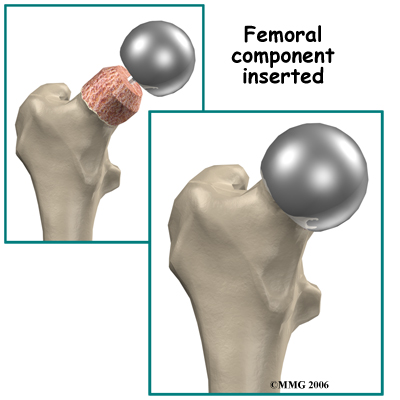
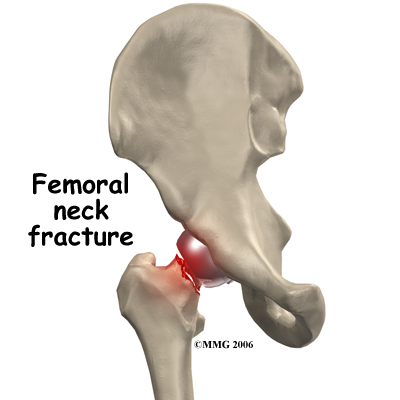
Fracture of the Femoral Neck
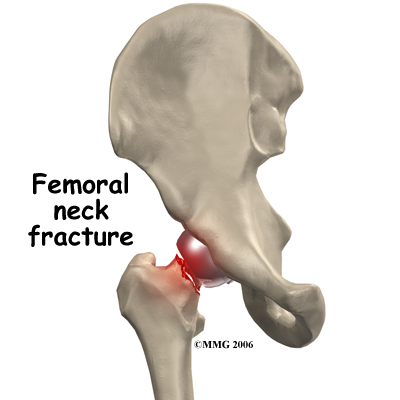
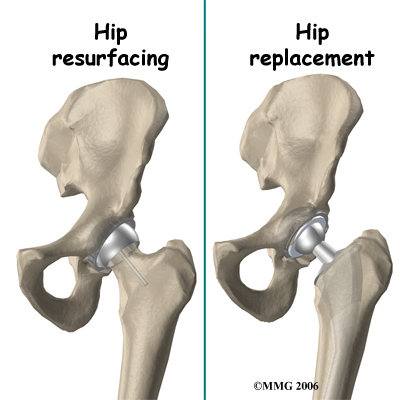
Fracture of the femoral neck is a unique complication of hip resurfacing. The replacement cap fits over the femoral head and ends just about where the femoral neck begins. This meeting point is an area of increased stress risk. Patient obesity, decreased bone mass, and surgical error are common risk factors in femoral neck fracture.
Leg Length Inequality
If there is any bone loss a difference in leg length can occur. When a surgeon does a traditional artificial hip replacement, the leg can be lengthened or shortened to match the other side. Because much less bone is removed during hip joint resurfacing, the surgeon cannot adjust the length of the leg. If you have a leg length difference before the procedure it will remain essentially the same.
After Surgery
What happens after surgery?
After surgery, your hip will be covered with a padded dressing. Special boots or stockings are placed on your feet to help prevent blood clots from forming. A triangle-shaped cushion may be positioned between your legs to keep your legs from crossing or rolling in.
If your surgeon used a general anesthesia, a nurse or respiratory therapist will visit your room to guide you in a series of breathing exercises. You'll use a breathing device known as an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
Physiotherapy treatments are scheduled one to three times each day as long as you are in the hospital. Your first session is scheduled soon after you wake up from surgery. Your therapist will begin by helping you move from your hospital bed to a chair. By the second day, you'll begin walking longer distances using your crutches. Most patients are safe to put comfortable weight down when standing or walking. However, if your surgeon used an uncemented prosthesis, you may be instructed to limit the weight you bear on your foot when you are up and walking.
Your therapist will review exercises to begin toning and strengthening the thigh and hip muscles. Ankle and knee movements are used to help pump swelling out of the leg and to prevent the formation of blood clots.
This procedure requires the surgeon to open up the hip joint during surgery. This puts the hip at some risk for dislocation after surgery. To prevent dislocation, patients follow strict guidelines about which hip positions to avoid (called hip precautions). Your therapist will review these precautions with you during the preoperative visit and will drill you often to make sure you practice them at all times for at least six weeks. Some surgeons give the OK to discontinue the precautions after six to 12 weeks because they feel the soft tissues have gained enough strength by this time to keep the joint from dislocating.
Related Document: Eastwood Physiotherapy's Guide to Artificial Hip Dislocation Precautions
Patients are usually able to go home after spending two to four days in the hospital. You'll be on your way home when you can demonstrate a safe ability to get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely, and consistently remember to use your hip precautions. Patients who still need extra care may be sent to a different hospital unit until they are safe and ready to go home.
Your staples will be removed two weeks after surgery.
Most orthopedic surgeons recommend that you have checkups on a routine basis after your joint resurfacing. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends.
Patients who have a joint implant will sometimes have episodes of pain, but if you have pain that lasts longer than a couple of weeks, you should consult your surgeon. During the examination, the orthopedic surgeon will try to determine why you are feeling pain. X-rays may be taken of your hip to compare with the ones taken earlier to see if there is any evidence of fracture or loosening.
Portions of this document copyright MMG, LLC.